When someone suddenly stops taking an opioid drug, the first symptoms of withdrawal can appear within hours. Withdrawal from short-acting opioids like heroin can start within 6 to 12 hours from the last use and can continue for 4 to 10 days. Longer-acting opioids like fentanyl take longer to leave the body, so withdrawal symptoms usually don’t emerge until 12 to 48 hours after last use and can last anywhere from 10 to 20 days. Ways to treat mild opioid withdrawal include increased water and vitamin intake, while more severe withdrawal may require medication-assisted treatment.
For many people, withdrawal is the most challenging barrier to recovery, because all its unpleasant symptoms make sufferers believe the only way to stop the pain is to use drugs again. Understanding the fundamentals of opioid withdrawal is a crucial step in preparing for treatment and long-term recovery.
What is Opioid Withdrawal?
Withdrawal is a collection of mental and physical symptoms that appear after someone stops or reduces their intake of an opioid drug. Opiates alter the way the brain reacts to pain, which is why they are so popular as painkillers. When taken in excess, however, these drugs also interfere with the brain’s reward system to produce a euphoric sensation or a “high” feeling.
When someone consumes an opioid in doses higher than recommended for therapeutic effects, the drug floods the brain with serotonin and dopamine, which the brain’s reward system produces naturally in small amounts. These neurochemicals create motivation to perform functions necessary for survival by releasing dopamine and serotonin in response to basic actions like eating and socializing.
When someone takes opiates frequently, the brain gets used to swimming in synthetic neurochemicals and stops producing dopamine and serotonin. Opioids remove the natural motivation for many of life’s daily tasks while making the brain dependent on these drugs for feelings of pleasure and reward. The brain also requires increasing levels of opioids to feel good, leading to drug cravings when the substance begins to leave the system. At some point, a person struggling with opioid addiction may keep taking them just to feel normal.
When someone stops using opioids, the brain has no way to compensate for the sudden disappearance of pleasure-inducing chemicals. The result is an array of withdrawal symptoms ranging from deeply unpleasant to potentially life-threatening, depending on the duration and severity of the addiction.
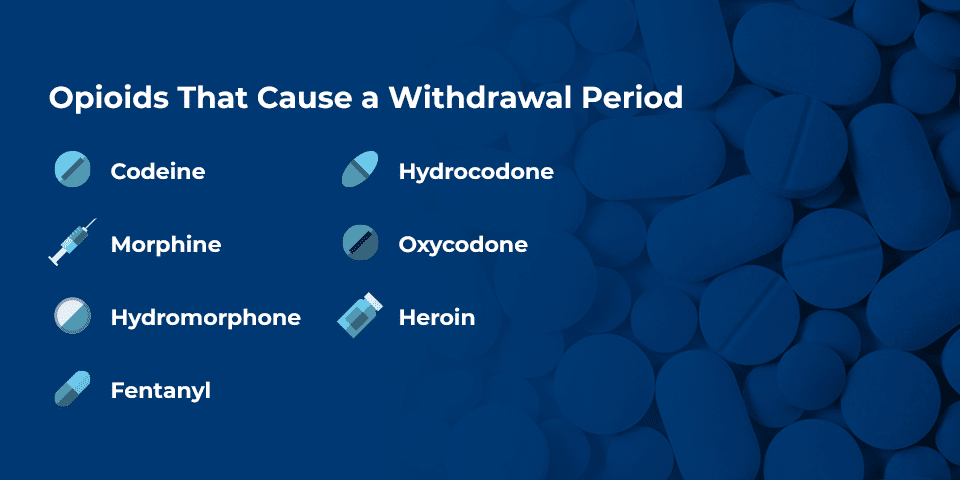
Opioids That Cause a Withdrawal Period
Any opiate can lead to withdrawal symptoms when someone suddenly stops using them. The range of opioids available through both legitimate and illegal channels is wide, and each drug varies in strength. Here are seven of the most common opioids that can cause a withdrawal period after cessation.
Codeine
Codeine is a medication used to relieve mild or moderate pain. It is available in tablet form, though most people get exposed to it through cough syrups with codeine as the primary ingredient. Despite its chemical similarities to stronger drugs like morphine and oxycodone, codeine is subject to fewer regulations. Its availability as medication also means some people who take it don’t realize its addictive potential.
Codeine can cause a person to feel unusually happy and calm, leading to drowsiness. It’s sometimes referred to by other names like “lean” or “purple drank” by recreational users. Frequent use can result in serious health issues, including seizures and hallucinations. Codeine withdrawal is usually somewhat less severe than other types of opioids, but it can always become more difficult the longer a person has misused it. Withdrawals generally begin 8-24 hours after last use and last an average of 4-10 days.
Hydrocodone
Hydrocodone, a key ingredient in Vicodin, is a semi-synthetic opioid analgesic used to treat moderate to severe pain. Drug manufacturers commonly pair it with acetaminophen in painkillers like Lortab. In 2014, doctors prescribed a total of more than 119 million medications with hydrocodone as an active ingredient. Doctors prescribe medications containing hydrocodone when other treatment options have not worked to curb injury-related pain.
These medications usually come in tablet form. Most prescriptions dictate one dosage every 4 to 6 hours, and this high frequency makes it easier to become addicted over time. It also means withdrawal symptoms set in very quickly after someone stops taking the medication. In the longer term, the worst of Vicodin withdrawal symptoms usually dissipate within 10 days of stopping usage and beginning treatment.
Morphine
Morphine is one of the oldest opiates and one of the only modern-day medications derived directly from the poppy plant. It is also a precursor to heroin and is highly dangerous. Physicians commonly use it to control patients’ pain before and after surgery, delivering it via an intravenous drip. It’s very easy to overdose when misusing liquid morphine due to its concentration. Although rare, morphine also comes in low-dose, extended-release tablets.
Morphine is highly regulated and difficult to obtain for most people. However, it is one of the drugs most likely for medical professionals such as nurses to misuse.
4. Oxycodone
Like hydrocodone, oxycodone is semi-synthetic, or human-made in labs with a combination of synthetic and natural components. Oxycodone is best-known brand names are Percocet and OxyContin. Oxycodone tablets were the second most common opioid prescribed in 2016, with 5 billion tablets distributed.
When taking oxycodone outside of a doctor’s prescribed limits, the potential for addiction is extremely high. Even when someone takes this medication according to the recommendations of their physician, it’s easy to build up a tolerance that transitions into dependence. Oxycodone is one of the most common prescription medications people struggle with abusing. OxyContin withdrawal symptoms are comparable to those of other opiates, but many people find detoxing from oxycodone more difficult because they get used to taking the medication every 4 to 6 hours.
Hydromorphone
This opiate is most widely available as a tablet to treat pain in those with severe chronic pain. Doctors only prescribe it to those who have already built up some tolerance from taking another opioid medication for at least a week. Hydromorphone is available in tablets and liquid, though tablets are more common. The brand Dilaudid is an immediate-release formulation of hydromorphone and the leading product for drug abuse containing hydromorphone.
Hydromorphone is chemically similar to oxycodone and hydrocodone, but scientists have found it to be moderately more potent than either of these counterparts. Most physicians prefer to prescribe hydrocodone or oxycodone due to their relatively lower potencies, but some still prescribe hydromorphone for patients who did not respond well to previous painkillers.
People who abuse hydromorphone do so because its injectable form is so concentrated and powerful. That also makes injectable hydromorphone much more difficult to detox from than the tablet form.
Heroin
Heroin is another opioid, but doctors do not prescribe it for any reason due to its extreme potential for addiction. This drug is derived from morphine and usually comes in a white powder or sticky black form known as “black tar” heroin. Heroin is significantly more potent than prescription opioids, as well as much cheaper. This combination leads to addiction more quickly than other opioids, and the fact that the drug is illicit doesn’t help.
Many people view heroin as the archetypal form of addiction, and it does come with many unpleasant physical side effects. Withdrawal from heroin is one of the most difficult among all opiates, and requires an unwavering commitment from the patient, in addition to expert treatment. While withdrawal from most opioids does not border on life-threatening, heroin addiction does need medication-assisted treatment or monitored detoxification due to the potential danger from dehydration during withdrawal.
Fentanyl
Fentanyl is a fully synthetic opioid designed to treat severe pain. Like morphine, medical professionals use fentanyl in its medicinal capacity to manage acute pain after surgery. However, fentanyl is between 50 to 100 times more powerful than morphine and is the most dangerous opioid currently available. Prescribed fentanyl comes in the form of shots, transdermal patches, or lozenges, but illicit fentanyl usually comes in powdered form.
The powdered form of fentanyl resembles cocaine and often ends up as a cutting agent to make low-grade street drugs more potent. Cocaine and heroin are common targets for the addition of fentanyl, as the three substances look similar enough to combine without detection. However, the people who consume drugs cut with fentanyl often don’t realize what they’re getting and are significantly more likely to overdose on the more powerful product. Those who don’t overdose are significantly more likely to become addicted, even if the primary drug they bought was not an opioid.
In 2016, synthetic opioids were involved in almost 50 percent of deaths, including possibly the most famous victim, musical icon Prince. Fentanyl is by far the most common synthetic opioid available on the black market. Fentanyl withdrawal is even more dangerous than heroin withdrawal, and people with a fentanyl dependency should not attempt to quit using it without medical supervision.
Common Opioid Withdrawal Symptoms
Withdrawal symptoms are one of the top reasons people go back to using opioids. The severity of withdrawal effects depends on how long someone has been misusing an opiate, and how potent the drug is. Codeine withdrawal is generally less strenuous than withdrawing from oxycodone, for example. However, a person who abused codeine for multiple years is likely to have more severe symptoms than someone who has misused oxycodone for one month. The symptoms of opiate withdrawal come in two stages. The onset of common opioid withdrawal symptoms, which usually begin within 24 hours after cessation, includes:
- Aching muscles
- Feelings of restlessness and anxiety
- Teary eyes
- Runny nose
- Insomnia
- Excessive sweating
The second wave of symptoms sets in within a day or so of the first. These effects make quitting cold turkey impossible even for the most determined individuals. These symptoms include:
- Prolonged goosebumps
- Nausea and vomiting
- Diarrhea and abdominal cramps
- Rapid heartbeat
- Heightened blood pressure
People struggling with substance misuse will experience varying intensities of every symptom, and not all withdrawals look the same. Severe addictions cause withdrawals that are more stressful for the brain and body, and no one should go through it alone. Seeking the help of a medical professional ensures these symptoms don’t damage the body or the chances of recovery.
What to Know About the Opioid Withdrawal Timeline
Knowing the approximate timeline and different stages of opioid withdrawal helps manage expectations for the start of recovery. Many people underestimate the discomfort they will experience, as well as the drug cravings withdrawal brings. To better envision the timeline, it helps to break down the four stages of opioid withdrawal.
Withdrawal Stage 1: 6 to 30 hours
Many people struggling with addiction experience some initial withdrawal symptoms without even realizing it. The runny nose, tiredness, and aching muscles that set in the first day after withdrawal are easy to mistake for a cold or flu. These symptoms mostly cause moderate discomfort at this stage.
Withdrawal Stage 2: 72 hours
Symptoms peak around three days after the last consumption of an opioid. At this point, the most dangerous symptoms set in, including rapid heartbeat and spiking blood pressure. This stage is when symptoms are at their most painful, and cravings at their absolute strongest. Most people who try to quit opioids alone fail during stage two due to the severity of the symptoms. With the most potent drugs like heroin and fentanyl, diarrhea and vomiting can lead to extreme dehydration if a person has no medical supervision.
Withdrawal Stage 3: One week
The most acute opioid withdrawal symptoms usually pass by the end of the first week of abstinence. Some of the initial effects remain, such as tiredness, aches, sweating and anxiety. Some people continue to experience nausea, and irritability is quite common. Cravings continue to be a central challenge during this period.
Withdrawal Stage 4: One month and beyond
After the first few weeks of withdrawal, most physical symptoms will cease or decline significantly. However, many people experience post-acute withdrawal syndrome (PAWS) for months as their brains re-calibrate to function without opiates. PAWS symptoms usually include anxiety, mood swings, tiredness, and insomnia. These symptoms are highly manageable with help from a counselor or other clinical professional.
The full opioid withdrawal timeline is longer than many people imagine when considering PAWS. A person in treatment needs a strong support system and ongoing therapy to maintain their recovery strides.
Questions to Confirm Opioid Addiction
It’s not always easy to determine if your opioid misuse has transitioned into addiction. If you’re concerned about your opiate use, ask yourself these questions to determine if you have an addiction:
- Am I spending time thinking about how to get more opioids?
- Am I considering or have I gone through black market channels for opioids?
- Is my work or school performance suffering?
- Am I losing interest in friends, family, and hobbies?
- Do I use opioids in inappropriate situations, such as during work or before driving?
If you answer yes to any of these questions and find yourself craving opioids, you’re likely contending with addiction.
Start Your Path to Recovery Today
Opiate addiction and withdrawal are deeply challenging to combat, but quality treatment makes long-term recovery possible. MedMark offers the best in substance abuse counseling and medication-assisted treatment — the two most effective tools to facilitate recovery. Our evidence-based, accredited programs provide the counseling and resources you need to succeed in treatment. If you’re ready to take the next steps and find out more, contact MedMark today.